This page is part of the FHIR Specification (v1.8.0: STU 3 Draft). The current version which supercedes this version is 5.0.0. For a full list of available versions, see the Directory of published versions  . Page versions: R5 R4B R4 R3
. Page versions: R5 R4B R4 R3
Work Group Clinical Decision Support  Public Health and Emergency Response Public Health and Emergency Response  | Ballot Status: n/a |
This draft of the CQF IG is being balloted as FHIR-Based Clinical Quality Framework (CQF-on-FHIR) as an STU ballot for the September 2016 ballot cycle. In addition, this guidance will be used to support the CQF-on-FHIR and Payer Extract tracks in the September 2016 FHIR connect-a-thon.
The guidance in this module is prepared as a Universal Realm Specification with support from the Clinical Quality Framework (CQF) initiative  , which is a public-private partnership sponsored by the Centers for Medicare & Medicaid Services (CMS) and the U.S. Office of the National Coordinator for Health Information Technology (ONC) to identify, develop, and harmonize standards for clinical decision support and electronic clinical quality measurement.
, which is a public-private partnership sponsored by the Centers for Medicare & Medicaid Services (CMS) and the U.S. Office of the National Coordinator for Health Information Technology (ONC) to identify, develop, and harmonize standards for clinical decision support and electronic clinical quality measurement.
The Clinical Reasoning module provides resources and operations to enable the representation, distribution, and evaluation of clinical knowledge artifacts such as clinical decision support rules, quality measures, order sets, and protocols. In addition, the module describes how expression languages can be used throughout the specification to provide dynamic capabilities.
Clinical Reasoning involves the ability to represent and encode clinical knowledge in a very broad sense so that it can be integrated into clinical systems. This encoding may be as simple as controlling whether or not a particular section of an order set appears based on the conditions that a patient has, or it may be as complex as representing the care pathway for a patient with multiple conditions.
The Clinical Reasoning module focuses on enabling two primary use cases:
To enable these use cases, the module defines several components that can each be used independently, or combined to enable more complex functionality. These components are:
These basic components can then be used to enable a broad variety of clinical decision support and quality measurement use cases, including knowledge sharing, decision support services, and clinical quality assessment and reporting. The topics below provide more detailed discussion on each of these components and uses:
| Topic | Description |
|---|---|
| Overview and Background | If you are interested in the background and development of the FHIR Clinical Reasoning module, this topic covers where it came from and why it exists. |
| Using Expressions | If you want to see how to add dynamic capabilities to FHIR resources using expressions, start here. |
| Definitional Resources | If you want to see how to describe definitional resources using the ActivityDefinition resource, start here. |
| Representing Knowledge Artifacts | If you want to represent knowledge artifacts such as Event-Condition-Action rules, Order Sets, or Protocols, start here. |
| Sharing Knowledge Artifacts | If you want to share and distribute knowledge artifacts, start here. |
| Clinical Decision Support | If you want to use the Clinical Reasoning module to provide or use Clinical Decision Support services, start here. |
| Quality Reporting | If you want to define or report clinical quality measures, start here. |
From the perspective of a Knowledge Author, this module describes an approach to representing knowledge artifacts within FHIR.
From the perspective of a Knowledge Content Provider, this module defines search functionality for using a FHIR server as a knowledge artifact repository.
From the perspective of a Knowledge Evaluation Service Provider, this module defines operations and profiles in support of evaluating quality measures, and defining a service for guidance request and response, consistent with the approach taken by the current Decision Support Service  specification.
specification.
And finally, from the perspective of a Knowledge Evaluation Service Consumer, this module defines the expected available operations and behavior of a knowledge evaluation service.
| Resource | Description |
|---|---|
| ActivityDefinition | A resource to represent definitional resources. |
| DataRequirement | A data type that represents a general data requirement for a knowledge asset such as a decision support rule or quality measure. |
| PlanDefinition | Represents the description of a plan for accomplishing a particular goal. This resource is used to represent a broad variety of clinical knowledge artifacts including decision support rules, order sets, and protocols. |
| Library | Provides a container for knowledge artifacts that includes logic libraries, model definitions, and asset collections. |
| ServiceDefinition | Describes a specific clinical decision support service and supports evaluation using the $evaluate operation. |
| GuidanceResponse | Represents the response to a specific guidance request returned by the $evaluate operation. |
| Measure | Represents a clinical quality measure and provides evaluation through the $evaluate-measure operation. |
| MeasureReport | Represents the response to a specific measure evaluation request returned by the $evaluate-measure operation. |
| Extension | Description |
|---|---|
| cqlExpression | A general purpose extension that supports the use of Clinical Quality Language within FHIR |
| fluentPathExpression | A general purpose extension that supports the use of FluentPath within FHIR |
| library | A general purpose extension that supports the declaration of dependencies that can be accessed by expression logic |
| qualityOfEvidence | An extension that can be applied to Attachments to indicate the quality of evidence in support of a particular artifact or recommendation. |
| strengthOfRecommendation | An extension that can be applied to Attachments to indicate the strength of a recommendation. |
| Profile | Description |
|---|---|
| CQIF-Questionnaire | Defines extensions to the base Questionnaire that allow it to be used as a DocumentationTemplate with behavior specified via logic in CQL libraries. |
Because Knowledge Artifacts are typically patient-independent, many of the resources in the clinical reasoning module have no patient security and privacy concerns beyond the normal sensitivity that should be paid in any electronic healthcare system environment. However, the evaluation use case, including decision support guidance request/response, as well as quality measure evaluation have significant patient security and privacy concerns.
For the clinical decision support evaluation use case, as with any patient-specific information, care should be taken to ensure that the request and response are properly secured both at rest and in-motion, and that all access to the patient's information is done via a properly authenticated and authorized mechanism. This is particularly true of decision support artifacts where the logic is ingested as part of the definition of the artifact. In this scenario, the evaluation engine must ensure that data access within the ingested logic is subject to the same authentication and authorization requirements as any other access.
For guidance services that receive patient information, ensure that logging and auditing trails do not inadvertently compromise patient privacy and security by logging potentially sensitive information in an unencrypted way. In addition, guidance and recommendations returned from the service must ensure that content that contains patient information is clearly indicated so that consuming clients can take the appropriate care in integrating and displaying the resulting guidance.
For quality measure evaluation, individual and patient-list reports have the potential to contain large amounts of patient information. As with the decision support guidance responses, care must be taken to ensure the patient information is only accessible to properly authenticated and authorized agents, and that inadvertent breaches are minimized by following appropriate logging and auditing protocols.
For more general considerations, see the Security and Privacy module.
| Use Case | Description |
|---|---|
| Providing a dynamic value for a resource element | Using expressions to define the value for an element of a FHIR resource. |
| Defining a CQL library | Using the Library resource to incorporate a Clinical Quality Language library for use in FHIR resources. |
| Defining a Model Definition artifact | Using the Library resource to incorporate the definition of an information model for use with expressions in FHIR. |
| Defining an Event Condition Action rule | Using the PlanDefinition resource to represent an event-condition-action rule in FHIR. |
| Defining a Referral Request activity | Using the ActivityDefinition resource to define a referral request activity that can be used as part of a knowledge artifact. |
| Defining a Medication Request activity | Using the ActivityDefinition resource to define a medication request activity that can be used as part of a knowledge artifact. |
| Defining an Order Set | Using the PlanDefinition resource to represent an order set. |
| Defining a Protocol | Using the PlanDefinition resource to represent a protocol. |
| Defining a Questionnaire with dynamic content | Using the Questionnaire resource and expression extensions to add dynamic functionality to a FHIR Questionnaire. |
| Defining a Service Module | Using the ServiceDefinition resource to define a decision support service module. |
| Obtaining guidance from a Decision Support Service | Using the $evaluate operation to request and process guidance from a decision support service. |
| Defining a Measure | Using the Measure resource to represent a clinical quality measure. |
| Evaluating a Measure | Using the $evaluate-measure operation to request calculation of a clinical quality measure. |
| Applying an ActivityDefinition | Using the $apply operation to realize the intent resource defined by an ActivityDefinition. |
| Applying a PlanDefinition | Using the $apply operation to realize a plan definition for a specific context. |
| Representing Quality of Evidence/Strength of Recommendation | Using the qualityOfEvidence and strengthOfRecommendation extensions to indicate ratings associated with evidence for a particular artifact or recommendation. |
The resources defined for the Clinical Reasoning module are the result of the combined efforts of multiple communities working on the shared goal of harmonized standards and specifications for clinical decision support and quality measurement artifacts. The current state of the module reflects changes incorporated both from previous ballots on the FHIR-specific material, as well as content derived from several other balloted specifications in the CDS and CQM domains. The content at this point is capable of supporting the two primary use cases of sharing and evaluation in both domains and for a broad variety of artifacts.
In particular, the use of Clinical Quality Language (CQL) as a foundational mechanism for representing clinical quality logic enables decision support and quality measurement artifacts to share common definitions. For example, a Chlamydia Screening measure and related decision support artifacts focused on improving the measure can share a common library that describes the criteria for detecting when Chlamydia Screening is required in a patient. The decision support rule applies these criteria to determine when and how to impact a workflow, while the quality measure uses this same criteria to determine whether the screening goal has been met for a patient or population. In addition, the resources defined in this module use common patterns for describing the structure of artifacts and their associated metadata, enabling a consistent approach to the sharing and distribution of clinical knowledge artifacts.
The goals of the module over the next year are to provide a stable basis for implementation of the sharing and evaluation use cases. The Clinical Quality Framework Initiative will use these resources as the basis for implementation projects, targeting an FMM level of 3 or 4 for all module resources within a year. We are actively seeking comments on all areas of the module, with particular focus on supporting the following scenarios:
The FHIR Clinical Reasoning module is sponsored by the Clinical Decision Support (CDS) and Clinical Quality Information (CQI) HL7 Work Groups, with input and coordination from the FHIR Infrastructure and Service Oriented Architecture HL7 Work Groups.
The Clinical Quality Framework initiative has focused on harmonizing the historically disjointed specifications used by the Clinical Quality Measurement and Clinical Decision Support communities. Specifically, the initiative has focused on the specifications used to represent knowledge artifacts within the two communities. The strategy employed has been to break the conceptual content of knowledge artifacts into three core components, to define common standards for these core components, and to re-use these common standards for both clinical decision support and clinical quality measurement:
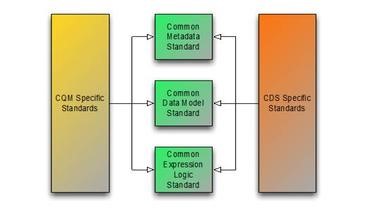
The first component has resulted in the Clinical Quality Common Metadata Conceptual Model  , an informative document harmonizing metadata requirements between Quality Measurement and Decision Support artifacts.
, an informative document harmonizing metadata requirements between Quality Measurement and Decision Support artifacts.
The second component has resulted in the QUICK Conceptual and Logical  Models, a harmonization of the Virtual Medical Record (vMR)
Models, a harmonization of the Virtual Medical Record (vMR)  used in Decision Support and the Quality Data Model (QDM)
used in Decision Support and the Quality Data Model (QDM)  used in Quality Measurement, and with its core requirements realized in FHIR as the Quality Improvement Core (QICore) profiles
used in Quality Measurement, and with its core requirements realized in FHIR as the Quality Improvement Core (QICore) profiles  .
.
Finally, the third component has resulted in the Clinical Quality Language specification  , a harmonization of the expressive capabilities of the Clinical Decision Support Knowledge Artifact Specification (CDS KAS)
, a harmonization of the expressive capabilities of the Clinical Decision Support Knowledge Artifact Specification (CDS KAS)  (produced by the Health eDecisions
(produced by the Health eDecisions  (HeD) Standards and Interoperability (S&I) initiative), and the Health Quality Measures Format (HQMF)
(HeD) Standards and Interoperability (S&I) initiative), and the Health Quality Measures Format (HQMF)  .
.
As part of the ongoing CQF initiative pilot efforts, these developing specifications are being used to support knowledge artifact sharing, as well as evaluation of knowledge artifacts as part of decision support request/response and measure evaluation.
This module continues the harmonization of quality domain specifications by defining an approach to using a FHIR server as a component of a knowledge system in both the Knowledge Repository and Knowledge Evaluation Service roles.
The approach and representations within this guide are derived from and intended to be consistent with the following specifications:




This material includes SNOMED Clinical Terms ® (SNOMED CT®), which are used by permission of the International Health Terminology Standards Development Organization (IHTSDO). All rights reserved. SNOMED CT was originally created by the College of American Pathologists. "SNOMED ®" and "SNOMED CT ®" are registered trademarks of the IHTSDO.
This material contains content from Logical Observation Identifiers Names and Codes (LOINC®) (http://loinc.org  ). The LOINC table, LOINC codes, and LOINC panels and forms file are copyright © 1995-2011, Regenstrief Institute, Inc. and the LOINC Committee and available at no cost under the license at http://loinc.org/terms-of-use
). The LOINC table, LOINC codes, and LOINC panels and forms file are copyright © 1995-2011, Regenstrief Institute, Inc. and the LOINC Committee and available at no cost under the license at http://loinc.org/terms-of-use  .
.
This material contains content from the Unified Code for Units of Measure (UCUM) (http://unitsofmeasure.org  ). The UCUM specification is copyright © 1999-2013, Regenstrief Institute, Inc. and available at no cost under the license at http://unitsofmeasure.org/trac/wiki/TermsOfUse
). The UCUM specification is copyright © 1999-2013, Regenstrief Institute, Inc. and available at no cost under the license at http://unitsofmeasure.org/trac/wiki/TermsOfUse  .
.
This material contains quality measure content developed by the National Committee for Quality Assurance (NCQA). The measure content is copyright (c) 2008-2013 National Committee for Quality Assurance and used in accordance with the NCQA license terms for non-commercial use.
| Project Facilitator/Editor | Bryn Rhodes | Database Consulting Group | bryn@databaseconsultinggroup.com |
| Project Facilitator/Editor | Jason Walonoski | The MITRE Corporation | jwalonoski@mitre.org |
| Editor | Marc Hadley | The MITRE Corporation | mhadley@mitre.org |
| Modeling Facilitator | Gay Dolin | Intelligent Medical Objects | gdolin@imo-online.com |
| Publishing Facilitator | Lloyd McKenzie | Gevity | lmckenzie@gevityinc.com |
| Domain Expert | Claude Nanjo | Cognitive Medical Systems | cnanjo@cognitivemedicine.com |
| Domain Expert | Esteban Aliverti | Cognitive Medical Systems | ealiverti@cognitivemedicine.com |
| Domain Expert | Chris Moesel | The MITRE Corporation | cmoesel@mitre.org |
| Domain Expert | Darrell Woelk | SocialCare | dwoelk@socialcare.com |
| Vocabulary Facilitator | Sarah Ryan | The MITRE Corporation | sarahryan@mitre.org |
| Vocabulary Facilitator | Rob McClure | MD Partners | rmcclure@mdpartners.com |
| Co-Chair | KP Sethi | Lantana Consulting Group | kp.sethi@lantanagroup.com |
| Co-Chair | Patricia Craig | The Joint Commission | pcraig@jointcommission.org |
| Co-Chair | Floyd Eisenberg | iParsimony LLC | feisenberg@iparsimony.com |
| Co-Chair | Chris Millet | National Quality Forum | cmillet@qualityforum.org |
| Co-Chair | Walter Suarez | Kaiser Permanente | walter.g.suarez@kp.org |
| Co-Chair | Guilherme Del Fiol | University of Utah Health Care | guilherme.delfiol@utah.edu |
| Co-Chair | Ken Kawamoto | University of Utah Health Care | kensaku.kawamoto@utah.edu |
| Co-Chair | Robert Jenders | Charles Drew University/UCLA | jenders@ucla.edu |
| Co-Chair | Howard Strasberg | Wolters Kluwer Health | howard.strasberg@wolterskluwer.com |